Crohn’s Disease
What is Crohn’s disease?
Crohn’s disease is an ongoing disorder that causes inflammation of the digestive tract, also referred to as the gastrointestinal (GI) tract. Crohn’s disease can affect any area of the GI tract, from the mouth to the anus, but it most commonly affects the lower part of the small intestine, called the ileum. The swelling extends deep into the lining of the affected organ. The swelling can cause pain and can make the intestines empty frequently, resulting in diarrheas.
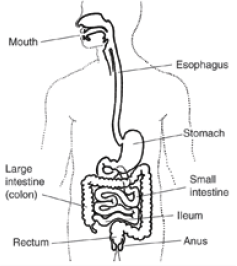
Crohn’s disease is an inflammatory bowel disease, the general name for diseases that cause swelling in the intestines. Because the symptoms of Crohn’s disease are similar to other intestinal disorders, such as irritable bowel syndrome and ulcerative colitis, it can be difficult to diagnose. Ulcerative colitis causes inflammation and ulcers in the top layer of the lining of the large intestine. In Crohn’s disease, all layers of the intestine may be involved, and normal healthy bowel can be found between sections of diseased bowel.
Crohn’s disease affects men and women equally and seems to run in some families. About 20 percent of people with Crohn’s disease have a blood relative with some form of inflammatory bowel disease, most often a brother or sister and sometimes a parent or child. Crohn’s disease can occur in people of all age groups, but it is more often diagnosed in people between the ages of 20 and 30. People of Jewish heritage have an increased risk of developing Crohn’s disease, and African Americans are at decreased risk for developing Crohn’s disease.
Crohn’s disease may also be called ileitis or enteritis.
What causes Crohn’s disease?
Several theories exist about what causes Crohn’s disease, but none have been proven. The human immune system is made from cells and different proteins that protect people from infection. The most popular theory is that the body’s immune system reacts abnormally in people with Crohn’s disease, mistaking bacteria, foods, and other substances for being foreign. The immune system’s response is to attack these “invaders.” During this process, white blood cells accumulate in the lining of the intestines, producing chronic inflammation, which leads to ulcerations and bowel injury.
Scientists do not know if the abnormality in the functioning of the immune system in people with Crohn’s disease is a cause, or a result, of the disease. Research shows that the inflammation seen in the GI tract of people with Crohn’s disease involves several factors: the genes the patient has inherited, the immune system itself, and the environment. Foreign substances, also referred to as antigens, are found in the environment. One possible cause for inflammation may be the body’s reaction to these antigens, or that the antigens themselves are the cause for the inflammation. Scientists have found that high levels of a protein produced by the immune system, called tumor necrosis factor (TNF), are present in people with Crohn’s disease.
What are the symptoms?
The most common symptoms of Crohn’s disease are abdominal pain, often in the lower right area, and diarrhea. Rectal bleeding, weight loss, arthritis, skin problems, and fever may also occur. Bleeding may be serious and persistent, leading to anemia. Children with Crohn’s disease may suffer delayed development and stunted growth. The range and severity of symptoms varies.
How is Crohn’s disease diagnosed?
A thorough physical exam and a series of tests may be required to diagnose Crohn’s disease.
Blood tests may be done to check for anemia, which could indicate bleeding in the intestines. Blood tests may also uncover a high white blood cell count, which is a sign of inflammation somewhere in the body. By testing a stool sample, the doctor can tell if there is bleeding or infection in the intestines.
The doctor may do an upper GI series to look at the small intestine. For this test, the person drinks barium, a chalky solution that coats the lining of the small intestine, before x rays are taken. The barium shows up white on x-ray film, revealing inflammation or other abnormalities in the intestine. If these tests show Crohn’s disease, more x rays of both the upper and lower digestive tract may be necessary to see how much of the GI tract is affected by the disease.
The doctor may also do a visual exam of the colon by performing either a sigmoidoscopy or a colonoscopy. For both of these tests, the doctor inserts a long, flexible, lighted tube linked to a computer and TV monitor into the anus. A sigmoidoscopy allows the doctor to examine the lining of the lower part of the large intestine, while a colonoscopy allows the doctor to examine the lining of the entire large intestine. The doctor will be able to see any inflammation or bleeding during either of these exams, although a colonoscopy is usually a better test because the doctor can see the entire large intestine. The doctor may also do a biopsy, which involves taking a sample of tissue from the lining of the intestine to view with a microscope.
What are the complications of Crohn’s disease?
The most common complication is blockage of the intestine. Blockage occurs because the disease tends to thicken the intestinal wall with swelling and scar tissue, narrowing the passage. Crohn’s disease may also cause sores, or ulcers, that tunnel through the affected area into surrounding tissues, such as the bladder, vagina, or skin. The areas around the anus and rectum are often involved. The tunnels, called fistulas, are a common complication and often become infected. Sometimes fistulas can be treated with medicine, but in some cases they may require surgery. In addition to fistulas, small tears called fissures may develop in the lining of the mucus membrane of the anus.
Nutritional complications are common in Crohn’s disease. Deficiencies of proteins, calories, and vitamins are well documented. These deficiencies may be caused by inadequate dietary intake, intestinal loss of protein, or poor absorption, also referred to as malabsorption.
Other complications associated with Crohn’s disease include arthritis, skin problems, inflammation in the eyes or mouth, kidney stones, gallstones, or other diseases of the liver and biliary system. Some of these problems resolve during treatment for disease in the digestive system, but some must be treated separately.
Which foods should I avoid with a Crohn’s disease diet plan?
The foods that trigger symptoms differ for each person with Crohn’s disease. To know which foods to leave out of your diet plan, you’ll need to determine which foods trigger yours. Many people with Crohn’s disease find that the foods on the following list aggravate symptoms during disease flares. So it’s likely that at least some of these listed foods will trigger your symptoms:
- alcohol (mixed drinks, beer, wine)
- butter, mayonnaise, margarine, oils
- carbonated beverages
- coffee, tea, chocolate
- corn husks
- dairy products (if lactose intolerant)
- fatty foods (fried foods)
- foods high in fiber
- gas-producing foods (lentils, beans, legumes, cabbage, broccoli, onions) • nuts and seeds (peanut butter, other nut butters)
- raw fruits
- raw vegetables
- red meat and pork
- spicy foods
- whole grains and bran
Once you’ve identified foods that cause your symptoms to flare, you can choose either to avoid them or to learn new ways of preparing them that will make them tolerable. To do that, you’ll need to experiment with various foods and methods of preparation to see what works best for you. For instance, if certain raw vegetables trigger a flare, you don’t necessarily need to give them up. You may find that steaming them, boiling them, or stewing will allow you to eat them without increased GI symptoms. If red meat increases fat in the stools, you could try eating ground sirloin or ground round to see if you can tolerate a leaner cut of beef. Or you might decide to rely on low-fat poultry without skin and fish as your main sources of protein.
Crohn’s Diet & Nutritional Supplements
For some it may be as simple as a change in diet, while for others it may require surgery. Nevertheless, expanding your understanding of this disease is the first step in over coming it. Throughout this article, you will find mentions of Eternal products as dietary supplements that has been included by many individuals as one of their standard treatment options for Crohn’s disease.
Suggested Approach to Crohn’s Diet
Inflammatory Bowel Disease IBD, including Crohn’s Disease and ulcerative colitis, is an inflammation of the intestines. These diseases cause the intestines to form ulcers and become inflamed, scarred and easy to bleed. The most common symptoms are diarrhea, acute abdominal pain, cramping, fever and fatigue. A special diet is very important in exercising IBD management to prevent malnutrition and extreme weight loss.
Nutritional Diet for Crohn’s Disease & Colitis
- Drink lots of fluid (8 – 10 servings daily) to keep body hydrated and prevent constipation.
- Your doctor or your registered dietitian may recommend a daily multivitamin mineral supplement (Wholefood according to blood group) to replace lost nutrients.
- Eat a high fiber diet when IBD is under control. Some patients find cooking and steaming the vegetables more tolerable than eating them raw.
- During a flare up, however, limit high fiber foods and follow a low fiber diet or even a low residue diet to give the bowel a rest and minimize symptoms. • Avoid lactose-containing foods such as dairy if you are lactose intolerant. Otherwise, you may use lactase enzymes and lactase pretreated foods. • It is very important to continue nourishing your body even during a flare-up. Try small frequent meals. Eating a high protein diet with lean meats, fish and eggs, may help relieve symptoms of IBD. Your registered dietitian may recommend pre-digested nutritional drinks (elemental diet) to give your bowel a rest and replenish lost nutrients so that your body can repair itself.
- Limit caffeine, alcohol and sorbitol (a type of sweetener) as these may exacerbate IBD symptoms.
- Limit gas-producing foods such as cabbage-family vegetables (broccoli, cabbage, cauliflower and brussels sprouts), dried peas and lentils, onions and chives, peppers and carbonated drinks.
- Reduce fat intake if part of the intestines has been surgically removed. High fat foods usually cause diarrhea and gas for this group of patients.
- If the ileum (part of the small intestines) has been resected, a Vitamin B12 injection may be required.
- Some studies found that fish oil (Man Yoo) helpful in managing IBD. Some also suggested the role of prebiotics such as psyllium in the healing process. Furthermore, probiotics (E-Probiotics) may also be helpful in aiding recovery of the intestines.
Eating right
Eating right is the key to good health for everyone. But it is especially important for people with Crohn’s, since the disease can deplete their bodies of essential nutrients. Just like everyone else, people with Crohn’s need to take in enough protein, calories, vitamins (A, D, C, B-12, and folic acid), minerals (calcium, iron, and zinc), and other nutrients to stay healthy.
To ensure that you are getting a sufficient amount of nutrients from your diet, it’s best to eat a balance of foods from the four food groups:
- Meat (or alternative sources of protein)
- Dairy
- Cereal and grains
- Fruits and vegetables
The key to formulating a diet that is right for you is paying attention to the way certain foods affect your body. If they seem to worsen your Crohn’s symptoms, eliminate them from your diet.
Vitamins and minerals
A person with Crohn’s may not get enough nutrients because the disease causes poor digestion and malabsorption of dietary protein, fat, carbohydrates, water, and essential vitamins and minerals. Your gastroenterologist or nutritionist may recommend adding a multivitamin or other dietary supplement, such as vitamin B-12 or folic acid, to protect against nutritional deficiencies and round out your diet. Crohn’s causes certain symptoms in your body that may deplete your body of essential nutrients.
The most commonly recommended vitamin supplements include vitamins B-12 and D and folic acid, while the recommended mineral supplements include calcium and iron. However, most people with Crohn’s benefit from simply taking a multivitamin regularly.
It is important to note that supplements should not take the place of food — they contain no calories — and that you should consult with your gastroenterologist before you begin taking any supplements.
The following table shows sources of important vitamins and minerals, though some foods may not be right for you. Be sure to talk to your doctor about a diet that is suitable for you.
| Nutrient | Source |
|---|---|
| Vitamin A | Liver, eggs, dairy products, fish liver oils, dark green leafy vegetables (e.g., green peas, spinach) |
| Vitamin D | Liver, fish liver oil, fortified food products (e.g., milk, butter, and cereals) |
| Vitamin C | Fruits (e.g., citrus fruits, bananas, apples) |
| Folic Acid | Liver, beets, corn, legumes, green leafy vegetables |
| Vitamin B-12 | Meat, fish, poultry |
| Calcium | Cheese, ice cream, milk, yogurt, sardines |
| Iron | Red meat, fish, poultry, eggs |
| Zinc | Animal protein (e.g., beef, chicken), plant foods, (e.g., legumes, bran, green peas) |


